Managing diabetes can often entail dealing with stress due to the numerous daily tasks involved in controlling blood sugar, taking medications, and preventing potential complications. During high-stress times, spikes in hormones, such as cortisol, can directly impact blood glucose levels, exacerbating diabetes control.
Thus finding healthy and constructive outlets for stress relief is vital — and nutrition represents one key area offering tangible solutions.
This article explores the interconnected relationships between stress, nutrition, and diabetes; evidence-based dietary strategies to simultaneously improve diabetes health and stress resilience; as well as lifestyle approaches for reducing anxiety. By arming yourself with these tools, you can significantly enhance your overall well-being.
How Does Stress Affect Blood Sugar Levels and Diabetes?
Under stressful conditions and “fight or flight” responses, the hormones cortisol, adrenaline, and glucagon are released, rapidly causing blood glucose to rise through multiple mechanisms:
- Breakdown of glycogen into glucose.
- Slowing insulin production.
- Resisting insulin efficacy.
- Stimulating gluconeogenesis.
Over time, chronic stress can lead to sustained high cortisol levels, which can worsen insulin sensitivity, increase inflammation markers, and accelerate diabetes progression.
Research shows strong correlations between various stress indices and poorer glycemic control. Those reporting higher stress have higher HbA1c levels on average:
| Lower Stress Group | Higher Stress Group | |
|---|---|---|
| Average HbA1c | 7.1% | 8.6% |
Similarly, major stressful events often precede a diabetes diagnosis. Effective stress relief is vital for optimum diabetes management.
Nutrition Strategies for Improving Diabetes and Stress
The good news is that evidence-based nutritional approaches can tackle both diabetes and stress simultaneously through key mechanisms such as:
- Controlling blood sugar without dramatic spikes and drops.
- Reducing inflammation underlying insulin resistance.
- Stabilizing energy and mood through steady nutrients.
- Promoting relaxation, sleep, and cognition via compounds that enhance GABA, serotonin, and acetylcholine signaling.
Sample Meal Plan
Incorporating nutrition to manage diabetes and reduce stress doesn’t have to be complex. Try this simple diabetes food delivery meal plan:
Breakfast: Oatmeal with berries and nuts; green tea.
Lunch: Veggie and chickpea salad; herbal tea.
Snack: Apple with nut butter; dark chocolate.
Dinner: Salmon with roasted veggies and quinoa; chamomile tea.
Dessert: Greek yogurt with cinnamon and walnuts.
Personalize Your Dietary Approach
While research supports certain dietary frameworks, individual needs vary. Monitor your blood sugar responses, energy levels, and stress markers while experimenting with different macronutrient ratios, meal timings, carb counts, etc., to personalize an optimal nutrition plan.
Tracking your mood alongside blood sugar levels can unveil valuable connections. Consider working with a professional for additional insights.
Cultivate Self-Care Rituals
Surround eating with mindfulness, self-compassion, and relaxation rituals to compound benefits. Calm the nervous system before meals, chew slowly, pause to appreciate flavors and sensations, take post-meal walks, and transition smoothly back to tasks. Small moments of purposeful relaxation help stress resilience accumulate.
Regulate Blood Sugars
To help control swings in glucose that exacerbate both diabetes and stress, be strategic with carbohydrate intake. Choose foods like non-starchy vegetables, nuts, seeds, legumes, berries, and minimally processed whole grains like steel-cut oats, quinoa, and farro that release energy slowly due to fiber and lower glycemic load.
Timed carb intake coordinated with medication peaks can also smooth sugar curves. Including adequate protein and healthy fats in your meals further stabilizes blood sugar by slowing digestion and providing sustained energy.
Try Anti-Inflammatory Diets
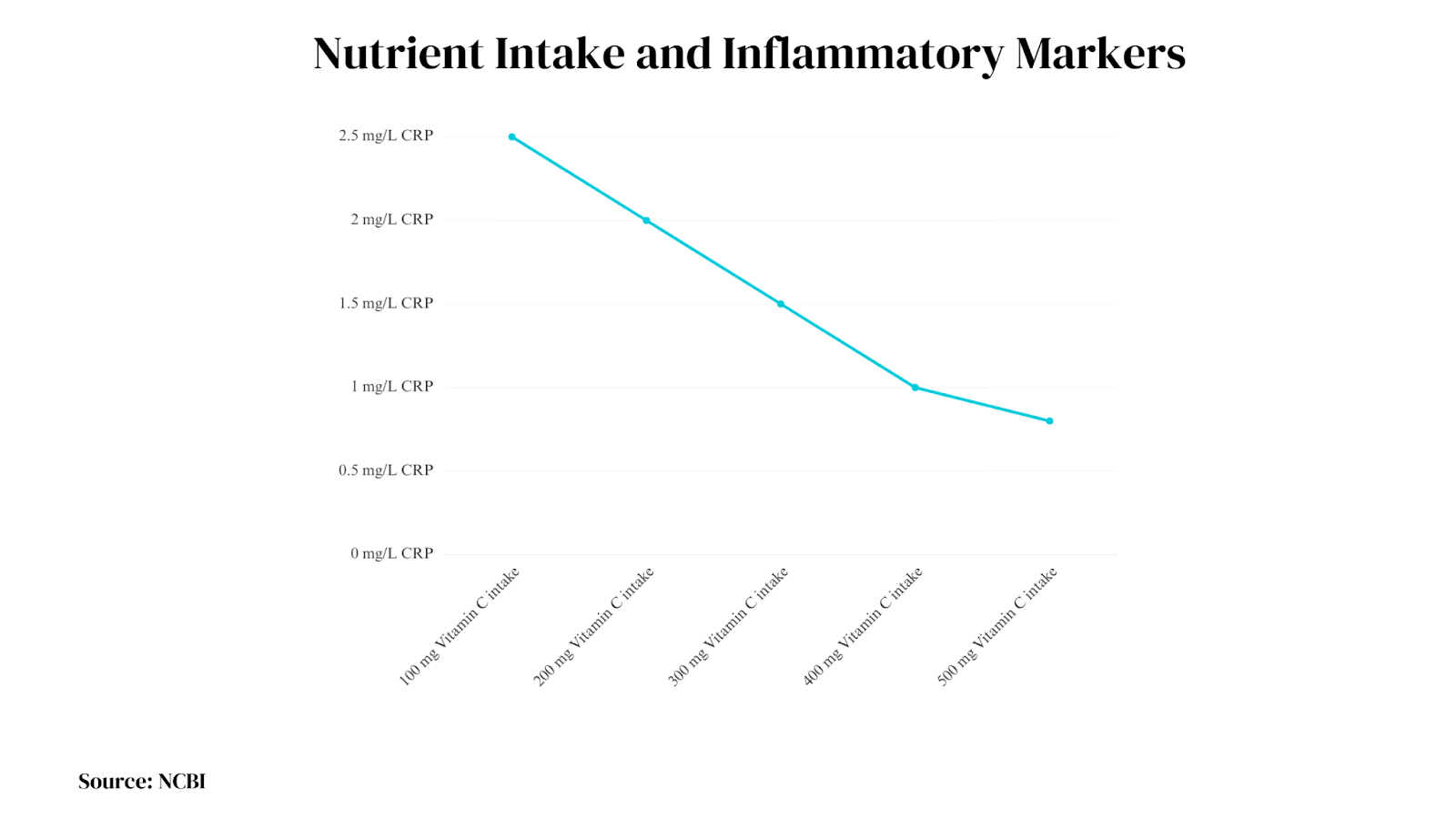
Chronic inflammation contributes substantially to insulin resistance, cardiovascular complications risk, and even anxiety pathways. Following evidence-based anti-inflammatory dietary frameworks can thus have wide-ranging benefits.
Diets rich in fruits, vegetables, legumes, whole grains, plant oils, fatty fish, probiotics, herbs/spices, and minimally processed foods consistently reduce inflammatory markers like hsCRP and pro-inflammatory cytokines tied to diabetes and mental health issues.
These anti-inflammatory diets avoid added sugars, refined carbs, and red meats. The Mediterranean diet and various plant-based approaches provide supported templates.
Data Source: NCBI
Ensure Adequate Nutrients
Getting sufficient amounts of key micronutrients enables the intricate biochemical pathways regulating not only healthy glucose metabolism and insulin sensitivity but also resilience against anxiety, low mood, and cognitive disturbances.
Critical nutrients include magnesium, zinc, chromium, vitamin D, antioxidant vitamins C and E, and B-vitamins like B6, B9, and B12 involved in neurotransmitter synthesis. Aim for whole food sources first, then address any ongoing gaps with targeted supplements in consultation with your healthcare provider and nutrition specialist.
Consider Stress-Reducing Compounds
In addition to adequate essential vitamins and minerals critical for reducing anxiety pathways, certain comforting whole foods contain unique bioactive compounds that directly improve relaxation signaling in the body and brain.
These include flavonoids like theobromine in dark chocolate, L-theanine in green tea, apigenin in chamomile, tryptophan in turkey and nuts, and cannabidiol in hemp products, among others. Working these edible stress relievers into your routine can provide tangible psychophysical boosts.
Additional Lifestyle Approaches
While nutrition forms the fundamental foundation, cultivating other positive lifestyle habits synergistically reduces stress and enhances diabetic outcomes.
Regular physical activity, restorative sleep, mindfulness practices like meditation, organizing systems and routines, meaningful social connection and support, professional mental health services, and overall self-care help manage the psychoemotional burden of diabetes over the long term. Using multiple evidence-based modalities in parallel empowers optimal wellness.
FAQs
What foods should I avoid when stressed with diabetes?
Avoid refined grains, added sugars, processed foods, and sugary drinks as these spike blood sugar and energy levels, then lead to crashes which exacerbate stress.
Are there specific carb limits I should follow when stressed?
Carb needs vary individually, but staying under 45% of total calories from carbs may help stabilize blood glucose during stress. Getting carbs from fruits, vegetables, and whole grains can further support stress management.
Which vitamin supplements help with both diabetes and stress?
Key micronutrients that can ease both conditions include magnesium, vitamin C, zinc, chromium, vitamin D, and B complex vitamins. Consult your healthcare provider for personalized advice.
By diligently focusing on nutrition and lifestyle, it’s possible to significantly reduce the dual burdens of diabetes and stress. This greater peace of mind and stabilized blood sugars will enable you to feel more empowered in your health journey.
Conclusion
In diabetes management, stress and blood glucose often feed off each other in a vicious cycle. However, research shows that targeted nutrition and lifestyle interventions can disrupt this connection for the better.
Working on controlling blood sugar fluctuations while addressing nutrient deficiencies that worsen anxiety represents a dual-pronged approach with significant potential to reduce HbA1c levels and enhance mental well-being.
By adopting healthier everyday eating strategies and incorporating stress-reduction habits, achieving a high quality of life while managing diabetes becomes more attainable.