It is no secret that our healthcare system is currently undergoing a significant crisis. And this is not new; this trend has been ongoing for some time now, exacerbated by the lingering effects of the pandemic. Facilities are facing pressures on all fronts, with rising operational costs, and staffing shortages are nationwide being just the tip of the iceberg.
An increasingly aging population, among both caregivers and patients, is adding to a widening gap between healthcare demand and workforce capacity.
As healthcare staff retire, without sufficient replacement, the pressure on the remaining workforce increases. Cuts in funding result in fewer hospital beds, more staff, and overall limited resources for facilities as they try to accommodate the rising demand.
Technology and Healthcare Innovation
Fortunately, technology is also advancing, helping to alleviate some of those difficulties. AI-driven workflows, direct-to-talent staffing platforms, or the use of wearables for client monitoring are making a huge difference. Together, these tools enable faster processes, provide wider access to care, and make qualified clinicians and caregivers available when they are needed most.
It is clear that healthcare innovation is a key solution to addressing today’s crises. However, as we examine the most significant challenges facing healthcare today and evaluate the available technological solutions, we must ask: Is it enough, and is it actually addressing the primary problems healthcare faces today?
The Biggest Challenges Facing Healthcare Today
To understand the efficacy of digital health solutions, we must first diagnose the severity of the condition. The healthcare sector is not merely struggling with inconvenience; it is facing structural threats that jeopardize patient safety and access to care.
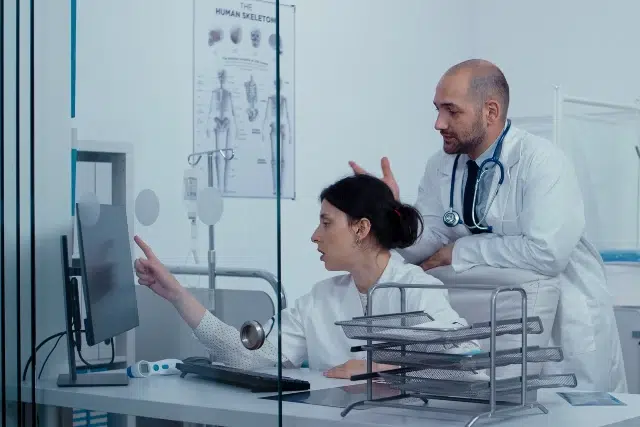
Staffing Shortages and Widespread Burnout
Across the United States, healthcare organizations face deep, persistent staffing shortages. Nurses, behavioral health specialists, primary care physicians, and specialty clinicians are in alarmingly short supply. A significant portion of the workforce is aging out, with accelerated retirements resulting from the emotional and physical strain of COVID-19.
Meanwhile, patient acuity has increased significantly, resulting in a higher workload per clinician. Under these conditions, hospitals have become dependent on overtime, supplemental contract labor, and costly travel nursing resources — further stretching budgets and staff morale.
Burnout is now recognized as a critical patient safety issue. Exhausted clinicians are more prone to errors, turnover rates rise, and patient satisfaction declines. Understaffing creates bottlenecks throughout the care continuum, resulting in delayed discharges, prolonged triage times, and slower throughput. These operational slowdowns negatively affect both the patient experience and hospital financial performance.
Patient Access Issues and Delayed Care
While demand for care continues rising, access remains a major barrier. Patients wait weeks or months for primary care visits, specialty consults, and mental health appointments. In rural and underserved regions, hospital closures and provider shortages create geographic care deserts, forcing patients to travel for hours to access routine services.
Under-resourced community hospitals struggle to keep up with demand, and limited appointment availability only worsens delays. When care is delayed, conditions often escalate, resulting in more severe illness — adding pressure to already strained systems.
Rising Costs and Operational Inefficiencies
Labor costs are climbing sharply as organizations rely on expensive temporary staffing to fill chronic gaps.
Operational inefficiencies are equally to blame for the financial bleed:
- Workflow Bottlenecks: Inefficient discharge processes create unnecessary length-of-stay extensions, occupying beds that incoming patients need.
- Administrative Waste: High rates of claim denials and complex coding requirements consume massive amounts of administrative time.
- Redundancy: Fragmented technology systems often generate duplicated efforts, where staff must perform the same task multiple times across different platforms.
Fragmented Systems that Don’t Communicate
Perhaps one of the most persistent barriers is the lack of seamless data exchange. Many electronic health records (EHRs) still cannot communicate with one another, preventing clinicians from accessing a comprehensive view of a patient’s medical history.
Inconsistent documentation standards between hospitals, specialty clinics, and primary care practices add to the difficulty. Broken information pathways — such as labs, imaging, or referral notes not syncing — force clinicians to manually re-enter or hunt down data. These gaps compromise safety, slow care, and frustrate both staff and patients.
How Technology is Addressing These Challenges
Despite these overwhelming obstacles, healthcare innovation is accelerating. New digital health tools, AI-driven systems, and streamlined workflows are enabling organizations to develop more efficient, equitable, and sustainable care models.
1. Telehealth Improving Access and Care Continuity
Telehealth has become essential for expanding patient access to healthcare. Virtual visits eliminate geographic barriers, allowing individuals in remote areas to connect with specialists without the need for lengthy travel.
Telepsychiatry is helping address widespread mental health shortages, while virtual primary care supports ongoing management of chronic diseases. Patients benefit from shorter wait times, and clinicians can triage more effectively. Telehealth also supports preventative health by making follow-up care easier to maintain.
2. Workforce Technology Improving Staffing Workflows
Healthcare facilities are increasingly adopting various technology-based tools to optimize schedules and workflows. To address the staffing crisis, facilities are shifting away from more rigid traditional solutions, such as staffing agencies, to the use of staffing technology with staffing marketplace platforms like Nursa. These platforms enable facilities to find qualified staff in real-time, eliminating the need for intermediaries and cutting overtime labor costs.
These platforms provide the following benefits:
- Speed and market demand dynamics: Instead of waiting days for an agency to manually source talent, schedulers can instantly post shifts in minutes and allow clinicians to request to fill them. This “Uber-like” efficiency helps facilities find reliable clinicians at their preferred rate, while handling sudden census spikes or last-minute call-outs.
- Automated credentialing: To protect patient safety, these platforms automatically verify licenses, background checks, and certifications before a clinician can book a shift. This ensures that every “instant” hire is fully vetted and Joint Commission compliant without adding administrative burden.
- Cost control: Unlike agencies with opaque margins, digital marketplaces offer transparent pricing where facilities control the hourly rate, significantly reducing the premium paid for contingent labor.
- Recruitment pipelines: Facilities can use per diem shifts as “working interviews,” vetting clinicians on the floor before offering full-time employment.
These components help care providers staff with more agility and establish a more resilient staffing strategy that meets both short- and long-term needs.
3. Remote Patient Monitoring Reducing Hospital Strain
Remote patient monitoring (RPM) tools such as Rimidi enable clinicians to track vital signs and symptoms remotely outside the hospital. This approach allows lower-acuity patients to stay safely at home, reduces unnecessary admissions, and shortens the length of stay by allowing for early discharge with virtual supervision.
For chronic disease management — such as heart failure, diabetes, and COPD — RPM supports preventative interventions before complications escalate. This not only improves outcomes for patients but also reduces hospital strain and overall costs.
4. EHR Improvements and Interoperability Gains
While challenges persist, EHR vendors and healthcare systems are making progress toward achieving interoperability. Centralized clinical dashboards, standardized data formats, and cross-system APIs are helping eliminate information silos.
The vision of a single patient record — accessible across hospitals, outpatient centers, and specialists — is becoming more realistic. These advancements boost efficiency and equip clinicians with the comprehensive insights needed for safer, more informed care.
5. AI and Automation Improving Clinical Workflow
AI in healthcare is shifting from future promise to daily practice. Intelligent automation is helping streamline administrative burdens such as prior authorizations, clinical documentation, and claims submission.
Natural language processing tools integrated into tools like Freed and Commure assist with note-taking, freeing clinicians from hours of manual charting. Predictive analytics flag high-risk patients, enabling earlier interventions.
Meanwhile, healthcare automation — from smart bed sensors to robotic medication dispensing — enables safer and more reliable operations. These innovations reduce errors, accelerate workflows, and free clinicians to focus on high-value care.
Persistent Challenges in Healthcare
While technology offers many benefits and fuels progress, major issues remain that technology alone cannot immediately fix:
- Data silos: Proprietary systems often restrict access to data, creating a barrier to effective collaboration. Without free-flowing information, providing seamless care across different providers is nearly impossible.
- Security risks: Bias and privacy concerns remain constant dangers. If AI models learn from historically biased data, the technology will naturally perpetuate those inequalities.
- Cost barriers: Advanced tech is expensive, causing smaller facilities to fall behind. Per diem staffing platforms provide a solution by lowering daily costs, freeing up the budget needed to adopt these new technologies.
- Digital divides: High-tech healthcare requires internet access and tech skills. This creates a gap that often excludes rural populations, seniors, and low-income patients
Healthcare must address these gaps collaboratively to ensure technology benefits every patient and provider.
The Future of Healthcare is Looking Bright
With the ongoing changes in political decisions regarding healthcare funding, from the unwinding of Medicaid to staffing mandates demanding minimum staffing ratios, problems persist and are unlikely to go away anytime soon.
So is technology in healthcare solving the largest problems?
Yes, but it is not a silver bullet. Slowly, technology is addressing data fragmentation with a shift towards unified “single patient records,” allowing clinicians to access patient records regardless of their specialty.
Meanwhile, workforce optimization in healthcare is becoming increasingly streamlined. Highly efficient staffing platforms provide fast and effective solutions that address not only staffing shortages and burnout but also rising costs and operational inefficiencies.
Similarly, AI and automation stand to significantly increase productivity across a number of applications. Little by little, technology is addressing healthcare’s largest obstacles, and while there is no magic fix, there is hope for a more efficient and accessible healthcare system.